
Costochondritis - Musculoskeletal Chest Pain
Costochondritis is a benign form of chest pain, in which pain arises from inflammation of joints between the ribs and the breast bone at the front of the chest. Suffers will often report a sharp or dull localised pain, that is often worse with certain movements and deep breathing. Nevertheless, as there is a long list of conditions (some more serious than others) that can cause chest pain, a physical examination is vital to rule out any involvement from the heart or lungs.
In a study by Disla, et al.(1), a group of 122 people presented to the emergency department with a complaint of chest pain. In this group, it was found that when you exclude those with fever, trauma or cancer, costochondritis accounted for 30% of the group’s pain. However, the main conditions your Health Practitioner must rule out are:
- Acute coronary syndrome
- Aortic dissection
- Pneumonia
- Pneumothorax
- Pulmonary embolism
- Rib fracture, if there was a recent fall or trauma

What is Costochondritis?
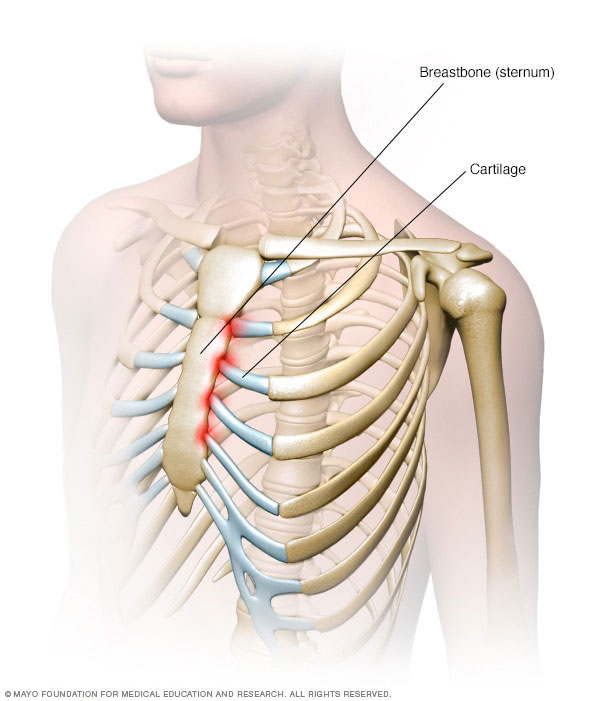
Each rib at the front of the body connects into the sternum (i.e. the breast bone) via a cartilaginous structure called the costal cartilage, as seen in the image below. This cartilaginous extension of each rib allows for greater flexibility of the ribcage, and hence increased elasticity to facilitate breathing. Costochondritis is when there is inflammation between the junctions of the costal cartilage and the sternum, most commonly seen at the 2nd to 5th ribs(2).
Costochondritis can occur after a large exertion, i.e. a heavy lift, or without any obvious injury(3). Often presents as a localised pain that worsens in certain positions of the trunk and deep breathing. Those afflicted by this condition, may also experience pain when pressure is applied directly onto the irritated joint. Conversely, this condition is normally not accompanied by radiating pain (down the arm), shortness of breath, dizziness, fever, cough, nausea, etc. – which can be signs of more worrisome cause of chest pain.
What do I do if I suspect I have Costochondritis?
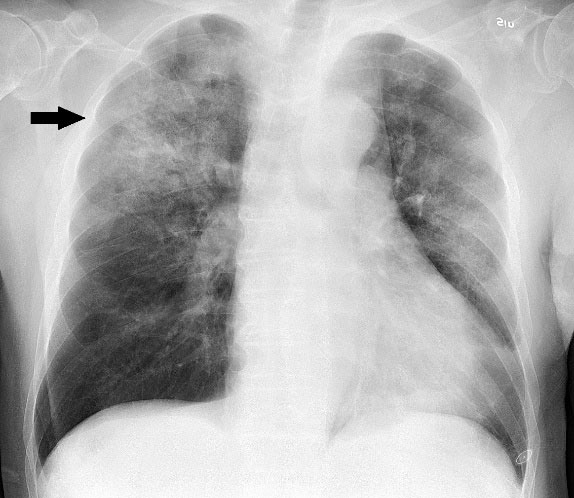
First and foremost, chest pain due to involvement of the cardiac or respiratory systems must be ruled. Primarily, this is the job of your General Practitioner – who can do a detailed check of vital signs as well as refer you onto relevant Medical imaging or investigations, such as chest X-Rays or ECG testing. Once we can be sure that there are no red flags, your Physiotherapist or Sports Chiropractor can assess for musculoskeletal causes of chest pain and begin treatment.
What does treatment involve?
Initially, the priority of costochondritis treatment is to reduce pain and disability – so that you’re able to get back to your everyday tasks. This may involve:
- Nonsteroidal anti-inflammatory (NSAID) medication
- Heat packs or anti-inflammatory gel – depending on personal preference
- Manual therapy and mobilisation
- Strategies to reduce trunk movement, such as quiet breathing and neutral sitting positions
Why costochondritis occurs in the first place is still being debated, however one popular theory is that it is muscle imbalances in the chest wall that lead to the development of this condition. As such, the next stage of treatment is active rehabilitation, to improve mobility and address any muscle deficits identified in your practitioner’s assessment. This includes gentle stretching, particularly of the pectoral muscles(3), and corrective exercises.

However, if an individual is suffering from long-standing costochondritis or they are finding their symptoms are significantly impacting their quality of life, your Physiotherapy or Sports Chiropractor may refer you onto a Sports Doctor. A Sports Doctor can assess whether a cortisone injection is needed to reduce pain in the short-term and facilitate rehab.
References:
1. Disla E, Rhim HR, Reddy A, Karten I, Taranta A. Costochondritis. A prospective analysis in an emergency department setting. Arch Intern Med. 1994 Nov 14;154(21):2466-9. PubMed PMID: 7979843.
2. Rovetta G, Sessarego P, Monteforte P. Stretching exercises for costochondritis pain. G Ital Med Lav Ergon. 2009 Apr-Jun;31(2):169-71. PubMed PMID: 19827277.
3. Costochondritis. (n.d.). Retrieved April 20, 2020, from https://www.physio-pedia.com/Costochondritis
4. Schumann JA, Parente JJ. Costochondritis. [Updated 2020 Jan 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532931/
