
ITB Syndrome
Iliotibial Band Syndrome, or ITB syndrome, is the most common cause of outer knee pain in the endurance-based athlete(1). In runners, it is estimated this condition will occur in 5-14% of the population(2), and in cyclists, ITB syndrome accounts for 15-24% of all injuries(1).
ITB syndrome is a non-traumatic overuse injury, which affect those involved in sports that require repetitive bending and straightening of the knee, such as: runners, cyclists, soccer players, tennis players, skiers and weight lifters(3). As such, this is one condition that rarely affects the less active.
Before we learn what causes ITB syndrome and its symptoms, it is important to first understand what the ITB or iliotibial band is.

The Iliotibial Band (ITB)
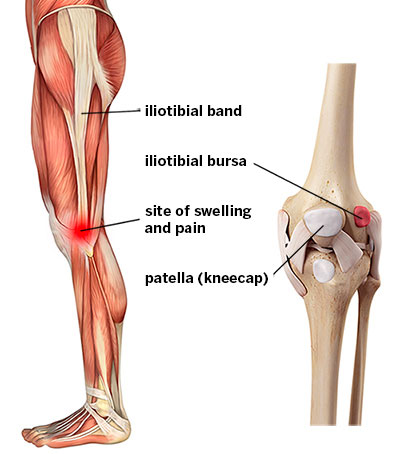
The ITB is a thick stiff band of connective tissue that runs along the length of the outer thigh. It starts near the outside of the hip bone, merging off the tensor fascia latae and gluteus max muscles. It then descends down the outer thigh and inserts into top of the tibia (i.e. the shin bone). This can be seen in the image above.
What causes ITB syndrome?
Due to where it attaches at the knee, the ITB has the potential to rub or “flick” over the outer prominence of the knee. In those training at high volumes, this repetitive friction of the ITB over the outside of the knee can lead to inflammation of the ITB, and hence pain.
What are the symptoms of ITB syndrome?
Those afflicted by ITB syndrome often report a sharp, burning pain on the outer aspect of the knee. Particularly for runners or field athletes, this pain may coincide with heel-strike and will be worse if running on a sloped surface or uphill. This may also be accompanied by an uncomfortable “flicking” or “snapping” sensation as the knee cycles through flexion and extension.
As the condition advances, sufferers may also notice their pain continues into rest after activity. Additionally, there may be exercise-related swelling and tenderness over this region as well.
Myths about ITB syndrome
1. Stretching and foam rolling reduces tightness of the ITB
False. The ITB is an incredible strong structure that is designed to be rigid and not to stretch. It does not have muscle fibres, so it does not have the capacity to contract and relax to change its length the way muscles do. As such, it is virtually pointless trying to stretch or foam roll the ITB itself.

However, there is some merit in improving the mobility of the musculature around the hip. In particular, the tensor fascia latae and gluteus maximus muscle attach directly onto the ITB. If you can improve the length of these muscles then you can help to reduce the tension of the ITB.
2. You need regular massage of the ITB to reduce pain
False. Similarly to our first myth, the ITB does not have the capacity to be “release”. Hence massage over the ITB will not improve its length.

3. ITB syndrome causes hip pain
False. ITB syndrome is called by repetitive rubbing over the bone prominence of the knee, strictly called the lateral femoral condyle. As such, the main location for pain will be the outer aspect of the knee, not the hip.
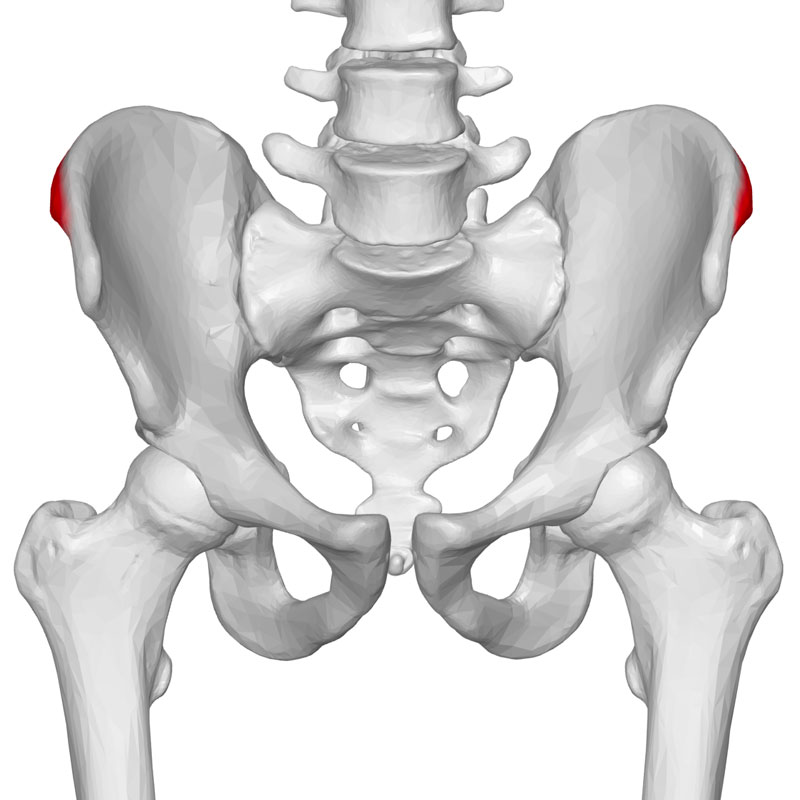
However, there is one instance where the ITB syndrome can pain above the hip, with some emerging evidence suggesting that the ITB can become strained at its insertion onto the crest of the pelvis. Cases of this type of ITB syndrome are quite rare and are usually seen in women who are physical active or overweight(4).
4. You may need surgery for ITB syndrome
False, active rehab with a Physiotherapist or Sports Chiro is always the best and first line of treatment for ITB syndrome. In particular, treatment may involve:
- Modifying training load
- Providing advice regarding footwear, training surfaces or symptom manage
- Corrective exercise to improve hip/knee coordination and running/cycling style
- Soft tissue release techniques to improve hip mobility (i.e. not “releasing” the ITB itself)
At present, there is very limited evidence to suggest those with ITB syndrome receive any benefit from surgical intervention(2).
References:
1. Ellis R, Hing W, Reid D. Iliotibial band friction syndrome--a systematic review. Man Ther. 2007 Aug;12(3):200-8. Epub 2007 Jan 8. Review. PubMed PMID:
2. van der Worp MP, van der Horst N, de Wijer A, Backx FJ, Nijhuis-van der Sanden MW. Iliotibial band syndrome in runners: a systematic review. Sports Med. 2012 Nov 1;42(11):969-92. doi: 10.2165/11635400-000000000-00000. Review. PubMed PMID: 22994651.
3. 17208506.Hadeed A, Tapscott DC. Iliotibial Band Friction Syndrome. [Updated 2019 Nov 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542185/
4. Sher I, Umans H, Downie SA, Tobin K, Arora R, Olson TR. Proximal iliotibial band syndrome: what is it and where is it? Skeletal Radiol. 2011 Dec;40(12):1553-6. doi: 10.1007/s00256-011-1168-5. Epub 2011 Apr 18. PubMed PMID: 21499978.
