
Tailbone Pain (aka Coccydynia)
What is the coccyx?
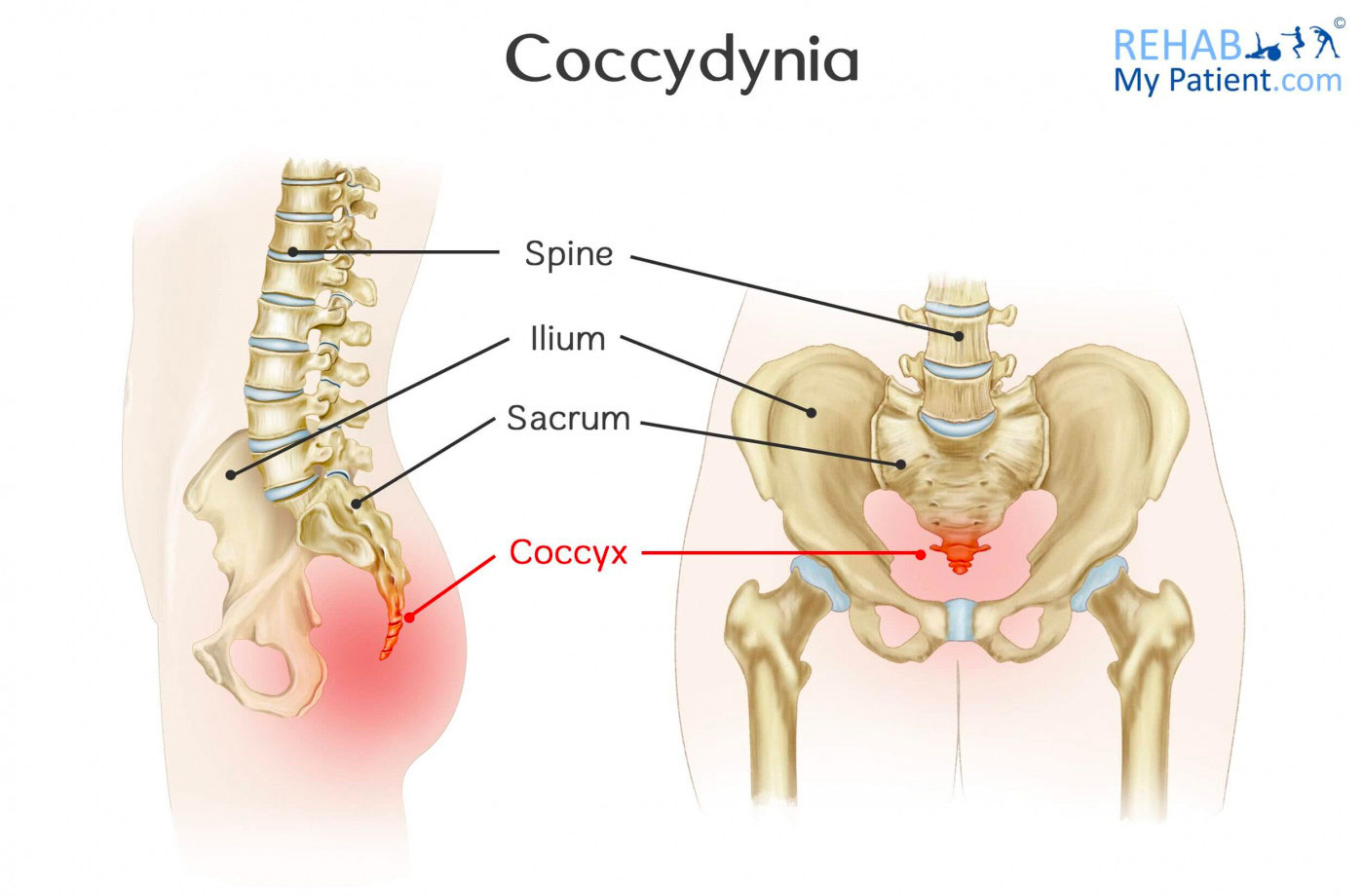
The coccyx (a.k.a. the tailbone) is a small bony wedged shaped structure located at the bottom of the spine. It technically consists of 3-5 separate vertebrae that are typically fused together to create a small curved triangular shape that resembles a shortened tail.
Despite its small size, the coccyx serves many important functions to the body. It provides a site of attachment for many muscles and ligaments, most notably the pelvic floor muscles and the gluteus maximus. It also creates a tripod formation with the pelvis, to provide support and balance when seated.
As such, Coccydynia is when pain arises from the region of the coccyx.
How does Coccydynia occur?
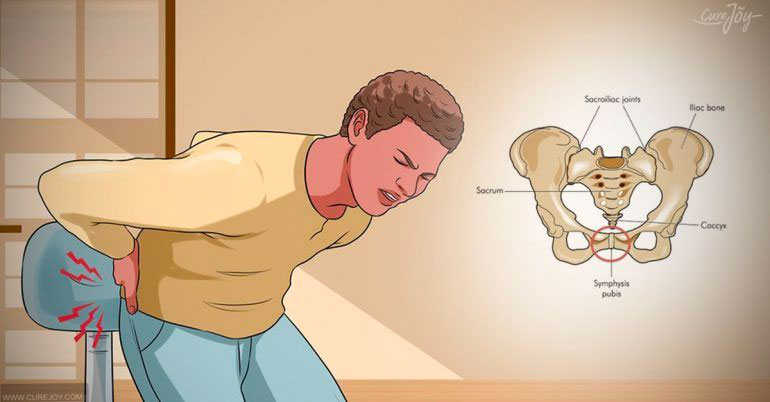
The most common cause of Coccydynia is direct trauma, which can be external or internal, and results in bruising, dislocation or fracture of the coccyx.
- External trauma usually involves a slip or fall back into the coccyx.
- Internal trauma usually occurs during childbirth. The coccyx is injured from the inside as the baby exits the birth canal. Use of delivery instruments, such as forceps, increase the risk of this type of injury.
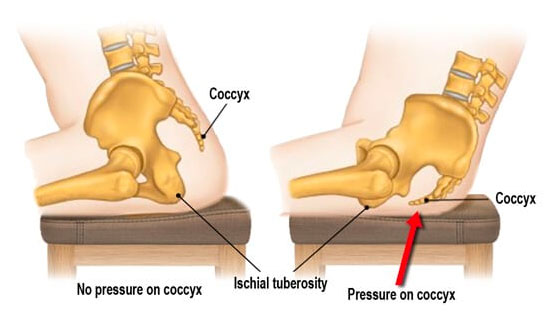
Acute trauma is the most common instigator of Coccydynia. However, this condition can also develop without an inciting injury but rather from repetitive or prolonged sitting on hard, narrow or uncomfortable surfaces(1). In addition, there has been anecdotal evidence to suggest rapid weight loss can also lead to Coccydynia due to a loss of mechanical cushioning. Structural changes, such as age-related joint changes or abnormalities in the laxity of the sacrococcygeal joint, can also contribute.
Although the trigger for Coccydynia is normally clean-cut – a distinct internal or external injury – the reason why coccyx pain persists even after the tissues are healed is less clear. Largely, it is true that inflammation of this bone and its joint, as well as contraction of the muscles attached to this bone, causes the characteristic Coccydynia pain. However, the possible factors leading to this inflammation are diverse(2). Most likely, it is more than one issue causing pain.
A practitioner must consider bony alignment and structure, multiple muscle groups, ligaments, and psychological influences when determining an effective treatment plan. They must also examine if the pain is referring from another region, including the spine (e.g. disc-related pain or nerve compression) or the neural tissue itself (i.e. neuropathic pain).
Symptoms of Coccydynia
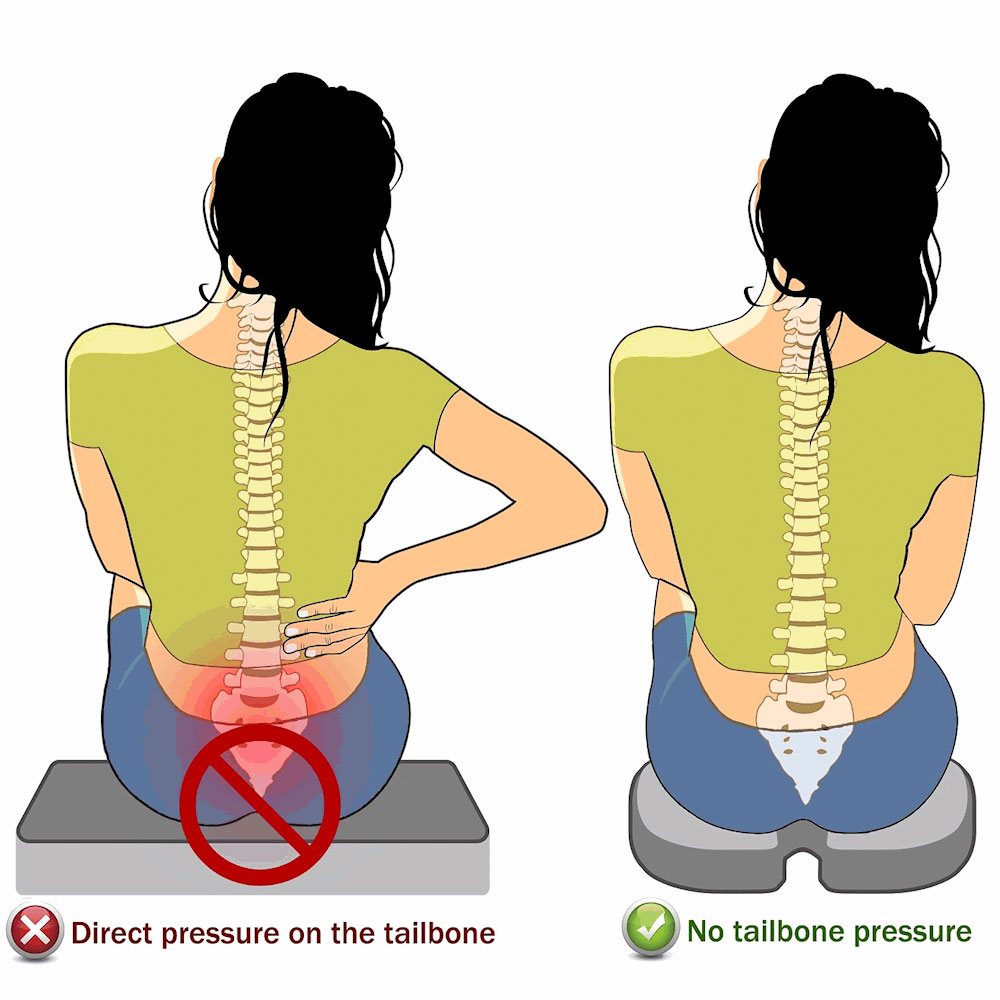
Although women are 5 times more likely to develop Coccydynia(1), this disabling condition affects both men and women. The hallmark symptom of Coccydynia is tenderness and pain localised over the coccyx, often accompanied by sensitivity of the adjacent muscles and soft tissue(3,4). These symptoms are usually worse in extended periods of sitting, standing or reclined positions. Furthermore, the act of transitioning from sitting to standing is a common aggravator.
Women with Coccydynia also report an exponential increase in pain during the premenstrual period, and occasionally pain during urination, defecation or sexual intercourse. This may be related to activation or spasm of the levator ani muscles, which composed the deep layer of the pelvic floor.
Treatment of Coccydynia
Due to the multifactorial nature of Coccydynia, best-practice management first requires a comprehensive clinical examination by a qualified practitioner, such as a Sports Chiro or Physiotherapist. In this, your practitioner can determine a plan to target the issues contributing to pain, as well as decide if a referral to a Specialist is required.
Conservative management is successful in approximately 90% of cases(5). Often this includes:
- Ergonomic modifications: to help offload the pressure on the coccyx, particularly when sitting. For example: strapping the buttock, postural changes or coccyx cushions.
- Manual therapy: including mobilisation of the coccyx and/or soft tissue release of the pelvic floor or surrounding musculature to address spasms or muscle tension.
- Corrective exercises: to improve motor control of the muscles that attach onto the coccyx or are affecting the way load is distributed through the pelvis or spine. This may include pelvic floor training.

In the rare cases that this has not been effective in alleviating pain, referral to a Sports Physician or Orthopaedic Surgeon may be indicated. Local injection of a steroid or local anaesthetic can be given, or furthermore, surgical intervention may be considered to remove the coccyx. Particular in traumatic cases, surgery has been shown to benefit those with persistent Coccydynia when all conservative methods have been unsuccessful (1,5,6).
References:
1. Pennekamp PH, Kraft CN, Stütz A, Wallny T, Schmitt O, Diedrich O. Coccygectomy for coccygodynia: does pathogenesis matter?. J Trauma. 2005;59(6):1414‐1419. doi:10.1097/01.ta.0000195878.50928.3c
2. Nathan ST, Fisher BE, Roberts CS. Coccydynia: a review of pathoanatomy, aetiology, treatment and outcome. J Bone Joint Surg Br. 2010;92(12):1622‐1627. doi:10.1302/0301-620X.92B12.25486
3. Schapiro S. Low back and rectal pain from an orthopedic and proctologic viewpoint; with a review of 180 cases. Am J Surg. 1950;79(1):. doi:10.1016/0002-9610(50)90202-9
4. Thiele gh. Coccygodynia: cause and treatment. Dis Colon Rectum. 1963;6:422‐436. doi:10.1007/BF02633479
5. Trollegaard AM, Aarby NS, Hellberg S. Coccygectomy: an effective treatment option for chronic coccydynia: retrospective results in 41 consecutive patients. J Bone Joint Surg Br. 2010;92(2):242‐245. doi:10.1302/0301-620X.92B2.23030
6. Capar B, Akpinar N, Kutluay E, Müjde S, Turan A. Koksidinili hastalarda koksiks eksizyonu [Coccygectomy in patients with coccydynia]. Acta Orthop Traumatol Turc. 2007;41(4):277‐280.