Posterolateral Corner of the Knee (PLC)
Does your knee feeling like its giving way or catching when you are walking?
The knee is a complex joint consisting of a capsule, ligaments, cartilage, tendons, and bony surfaces that keep the femur aligned with the tibia. The Posterolateral Corner (PLC) of the knee is an inherently important component in both knee function and stability. The PLC of the knee has 28 components of which each has a critical role in preventing hyperextension and varus (or outwardly directed) forces through the knee. An isolated injury to the PLC is uncommon, more likely this injury is coupled with ligamentous injuries such as the dreaded ACL, PCL injuries or tibial plateau fractures. Early diagnosis and management of this condition is key to successful repair or reconstruction if it is required. When surgery is not required, the benefit of conservative management is dependent on the severity and timing of the injury. The need for surgery or convective management will be best determined by a practitioner.
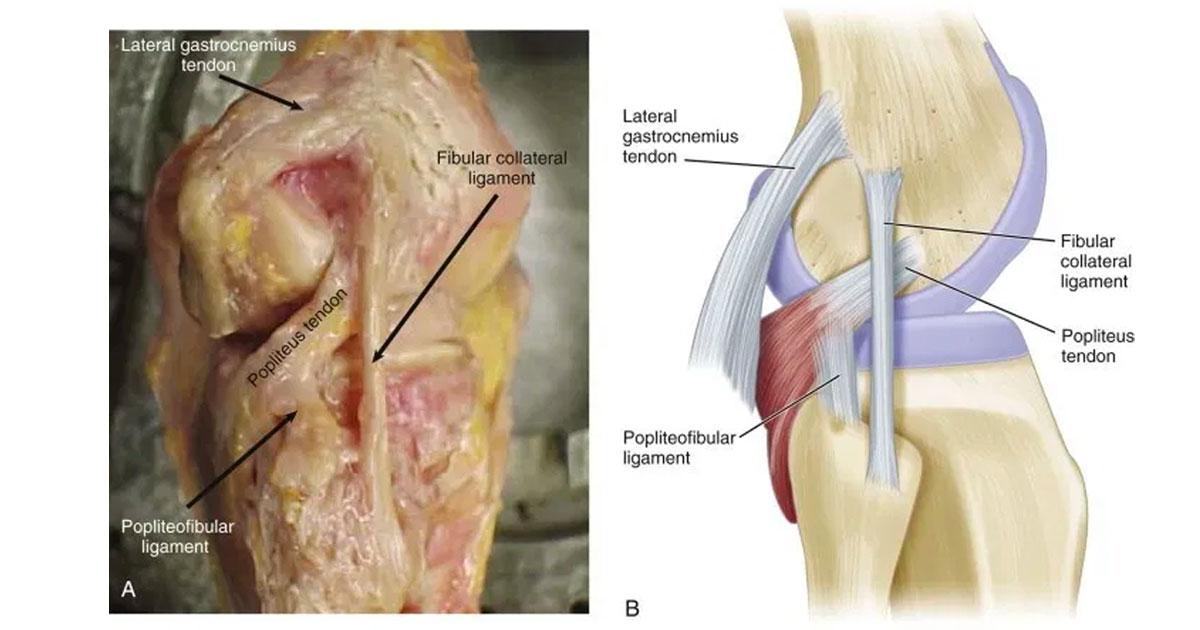
Anatomy of the knee:
The PLC is crucial to the stability of the knee at angles of less than 45° knee flexion (bending) during weight-bearing. The three most important structures of the PLC includes the popliteus tendon, popliteofibular ligament and fibular collateral ligament.
- The Popliteus tendon acts as a static and dynamic stabiliser against knee external rotation.
- The Popliteofibular ligament assists with resisting varus stress and is considered the primary restraint for external rotation forces at the knee. It is regarded as a crucial stabiliser to the PLC and is typically surgically reconstructed when torn.
- The Fibular collateral ligament From 0-30 degrees knee flexion the primary static stabiliser to varus opening.
Other structures which are important to consider are the posterolateral joint capsule, coronary ligament, oblique popliteal ligament and fabellofibular ligament also contribute to static stability of the PLC. Many of the static stabilising ligaments are a thickening of the capsule. The posterolateral joint capsule surrounds the knee like a blanket which the ligaments support.
Mechanism
The most common cause of a PLC injury is driven by a sports-related trauma, motor vehicle accident or a fall. The PLC is commonly injured with other ligamentous injuries of the knee, which can occur through knee hyperextension, external rotation and varus rotation. This can occur through knee dislocation or backwards directed force to the tibia.
Symptoms
The resulting instability of the knee is one of the key determinants of severity in a PLC injury. Instability in the knee commonly presents as the feeling of giving way, collapsing, painful clicking to clunking. Acutely an individual would typically complain of pain and swelling in the back and outside of the knee (posterolateral aspect). Once swelling and pain have subsided, symptoms of instability may be more evident, for example: buckling of the knee into hyperextension and varus when standing.
A PCL injury may also be accompanied by neurological compromise to the peroneal nerve which provides sensation and motor control to the outside of the calf. This has been reported in 30% in patients. This likely indicated an increased grade of ligamentous injury, as this type of deficit is commonly seen with disruption of the LC ligament and biceps femoris muscle tendon. Neurological symptoms from peroneal nerve injury include numbness, weakness or pins and needles. Chronic injuries of the PLC may present with inside or outside joint line pain with associated posterolateral pain. Knee extension (straightening) typically brings on instability symptoms such as locking and catching. Patients frequently feel knee hyperextension or locking with ascending and descending the stairs, and during a sport, movements that elicits symptoms of giving way include twisting, pivoting or cutting. Instability can occur in an acute injury or may develop over time with suffers from gene vacuum or concomitant cruciate ligament injuries.
Treatment
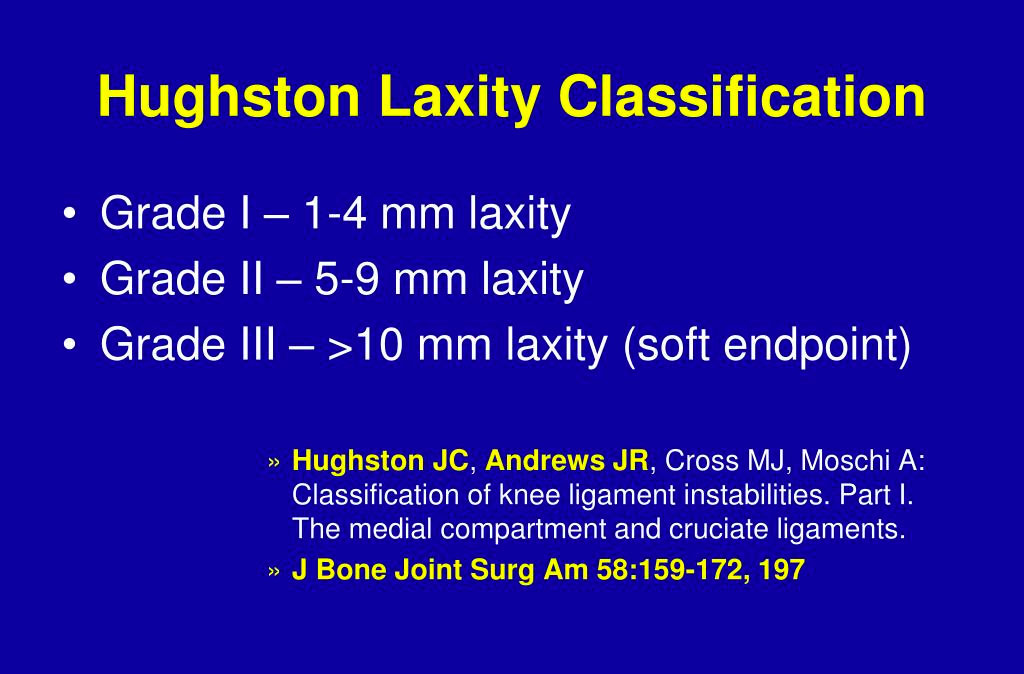
The treatment for PLC injuries is governed by the timing of the injury and severity. Grade I and moderate grade II can be treated conservatively with favourable results (explained in the diagram above - Hughston Laxity classification). However, surgical management of more severe grade II and all grade III injuries of the PLC is recommended, as non-operative management has led to poor functional outcomes. This includes residual laxity (loose muscle or limb) and progression to articular cartilage and meniscal degeneration. If surgery is deemed necessary then early intervention is crucial. Surgery is generally more successful in acute injury.