
Osgood Schlatter’s Disease
Osgood Schlatter’s disease is one of the most common causes of knee pain in the adolescent athlete. It is an overuse injury common in children who are highly active, particular in sports involving running and jumping such as basketball, volleyball, sprinters, gymnastics and football1. It affects 11.4% of boys and 8.3% of females1, and usually coincides with an adolescent growth’s spurt. That is, boys between the ages of 10 to 15years old and girls from 8 to 13 years old1. Furthermore, in about 20-30% of cases both knees will be affected(1).
What does Osgood Schlatter’s look like?
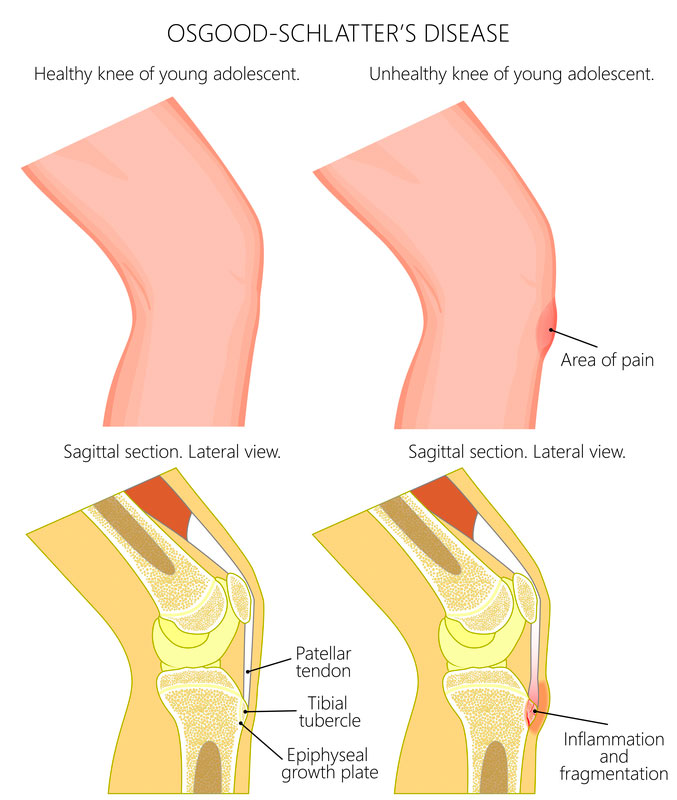
Children who develop Osgood Schlatter’s will complain of a painful bump on the front of the shin bone, where the quadriceps tendon attaches. This may be accompanied by redness or swelling over this bony prominence and loss of quadriceps muscle strength or muscle bulk. Moreover, this pain will worsen in physical activity, such as during or after playing sport, and will ease with rest(2).
What causes Osgood Schlatter’s?
Osgood Schlatter’s occurs when there is a discrepancy between muscle and bone length – that is, the lengthening of the quadriceps muscle can’t keep up with the lengthening of the femur bone1. Consequently whenever we contract our quadriceps muscle, such as in jumping or kicking, there is an increased traction of pull of the muscle at its bony attachment. This repeated micro-trauma irritates the bone and leads to tenderness and swelling at the front of the shin bone.
Other factors that predispose a children to Osgood Schlatter’s includes poor flexibility of the quadriceps and hamstring muscles, or misalignment of the knee-cap and connected tendons(1).

How do we treat Osgood Schlatter’s?
As Osgood Schlatter’s is largely related to growth spurts, this condition mostly resolved by itself once the skeletal system matures. Symptoms may persist up to 2 years but pain beyond this point is quite rare with only 10% of cases continuing(1). Furthermore, its importance to consider that there is no evidence linking volume of activity to degree of pain or continued activity with delayed recovery(2). This means decision to continue with sport and activity is up to the child and parent, as it depends on the individual’s symptoms and comfort levels.
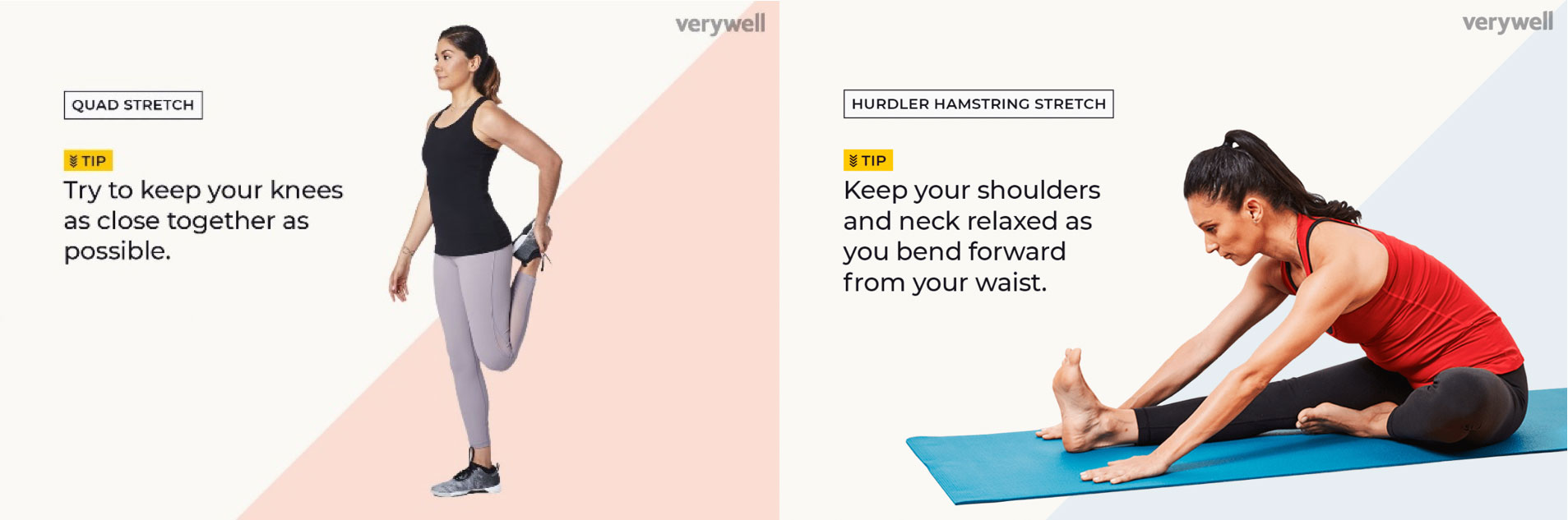
However, once diagnosed with Osgood Schlatter’s it is recommended to engage in a rehab program to stretch and strengthen both the hamstring and quadriceps muscles(3). Furthermore, there are many pain relief strategies that may help a child continue playing the sport they love. This includes pre-game stretching of the hamstrings and quadriceps muscles, and post-game ice application oral anti-inflammatories to minimise pain(3).
References
1. Smith JM, Varacallo M. Osgood Schlatter's Disease (Tibial Tubercle Apophysitis) [Updated 2019 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441995/
2. Landry M. (2014). Brukner & Khan's Clinical Sports Medicine. Physiotherapy Canada, 66(1), 109–110. doi:10.3138/ptc.66.1.rev2
3. Osgood Schlatter syndrome. (2019). Retrieved 3 September 2019, from https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/osgood-schlatter-syndrome
