
Gluteal Tendinopathy
You may not have heard of Gluteal tendinopathy, but you’ve probably heard of gluteal bursitis, trochantertic bursitis and greater trochantertic pain syndrome. At the end of the day, all these names describe the same phenomena; pain over the side of the hip with or without referral down the thigh, and pain that worsens in standing, walking, and climbing stairs. These are the people that can’t sit cross legged and sleep on their side with a pillow between their legs.
You may have near of Gluteal tendinopathy, or any one of its aliases, as over the age of 50 this condition afflicts 24% of women, almost 1 in 4! However, in men it is not nearly as prevalent, affecting 4times more women than men. Why it affects more women than men is due to a number of factors – such as bony alignment, issues with pelvic stability and gluteal strength – which we will discuss a little later.
What is Gluteal Tendinopathy?
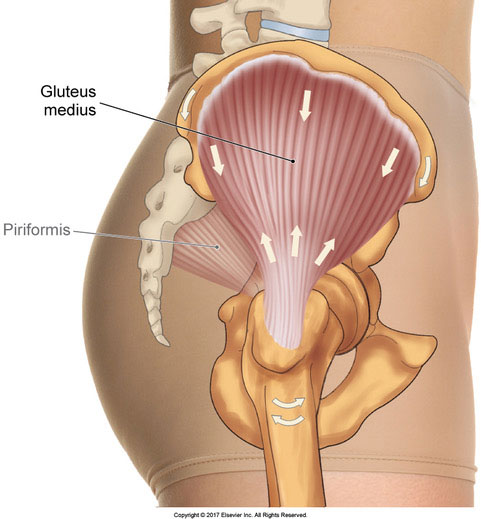
Gluteal tendinopathy occurs when there is a break-down of tendon tissue, specifically the fibrous band that connecting our smaller gluteal muscles (minimus and medius) to their attachment on the bony aspect of our hip (called the greater trochanter). Often pain will develop gradually overtime without any clear mechanism, and as it develops it becomes progressively difficult to walk or even sleep at night due to pain.
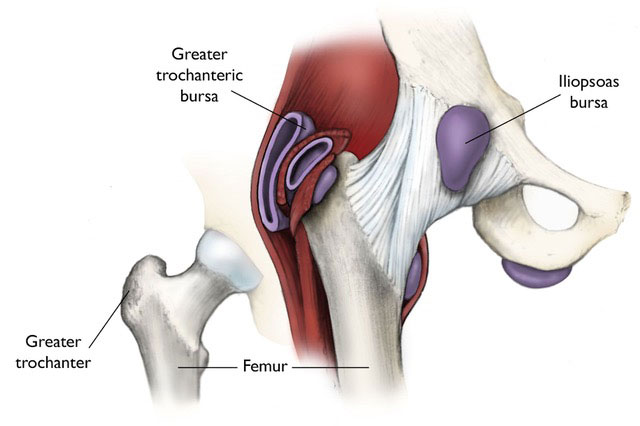
Traditionally, it was thought pain was due to inflammation of the bursae of the hip, little fluid filled sacs that lubricate between muscles and bones. However, research has shown only 20% of Gluteal Tendinopathy suffers have any sign of bursa irritation on medical imaging. Rather, the true culprit, in the large majority of cases is the tendon itself, hence lending to the name “Gluteal Tendinopathy”. Specifically, it’s the deeper portions of the tendon that becomes disrupted as it rubs over the bony prominence of the hip.
What causes Gluteal Tendinopathy?
Due to the hip’s unique structure, the specifics of what causes Gluteal Tendinopathy can be attributed to a number of factors that we may not see in other tendinopathies, such as in the tennis elbow or runner’s knee.
1) Glute strength
The root of any Gluteal Tendinopathy is strength, but rather of the smaller gluteal minimus and medius. These muscles are “abductors” muscles connecting the pelvis to the thigh, which means they help to lift up the leg sideways away from the body. But if we think of this system when our foot is planted, the reverse happens, our pelvis lifts up. Hence these muscles are crucial for hip stability, i.e. the ability to keep our pelvis level during single leg activities.
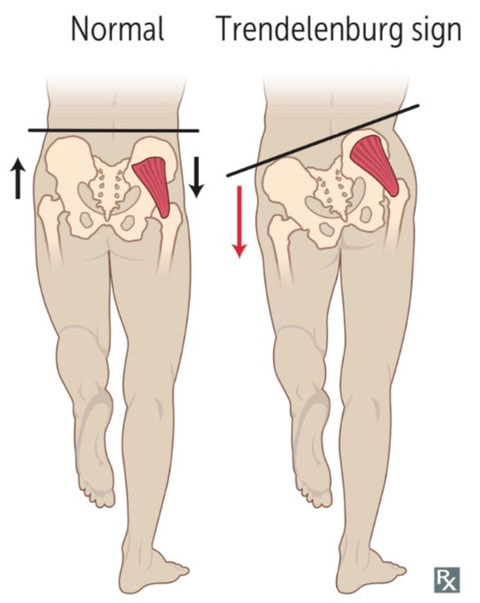
When these muscles aren’t quite strong enough they don’t provide adequate pelvic stability. As clinicians, we often see this as a hip drop pattern (also called Trendelenberg’s sign). As our hip drops down it compresses the minimus and medius muscle tendons against the bony prominence of the hip. As a result, the tendon fibres can thin and tear as it rubs over the bone again and again.
Adapted from Grimaldi et al., 2015 (1)
2) The structure and alignment of our hip bones
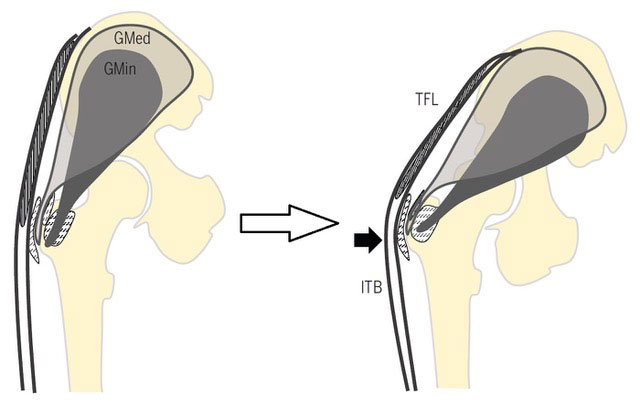
Unfortunately, this is another one of those times where it pays to be a man. As women’s pelvis and hips are built for childbirth, there are 2 key differences that are structurally different between a male and female pelvis (as shown below).
- Women’s pelvis are naturally wider and shorter
- Women’s femurs (the thigh bone) normally have a greater degree of bend at the top
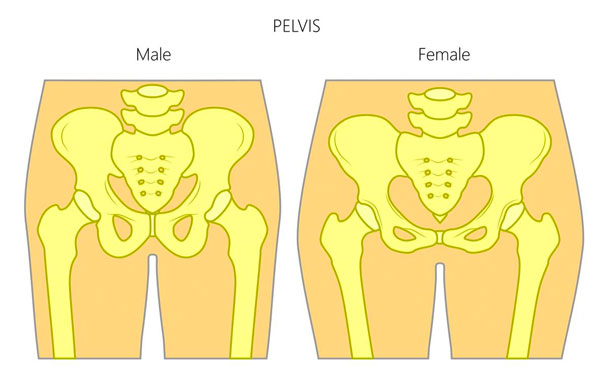
What this means is that women are genetically predisposed into having poor gluteal strength (as our muscles have less mechanical advantage) and greater compressive forces on the gluteal tendons (as the angle the muscles wrap around is sharper). Unfortunately, these are the main 2 mechanisms for the development of Gluteal Tendinopathy.
However, it’s important to remember that just because women are at greater risk of developing Gluteal Tendinopathy does mean that this is normal. Like most musculoskeletal problems, Gluteal Tendinopathy is very treatable in men and women alike, and shouldn’t be put down to an inevitability of aging.
References:
1. Grimaldi A, Fearon A. Gluteal Tendinopathy: Integrating Pathomechanics and Clinical Features in Its Management. J Orthop Sports Phys Ther. 2015 Nov;45(11):910-22. doi: 10.2519/jospt.2015.5829. Epub 2015 Sep 17. Review. PubMed PMID: 26381486.
