
Benign Paroxysmal Positional Vertigo
What is BPPV?
BPPV is a condition of the vestibular system which involves episodic dizziness caused from calcium carbonate crystals in the inner ear becoming dislodged and out of normal position. These crystals are commonly dislodged from the utricle of the inner ear and then travel into the semicircular canals/ducts.
Of all the affected canals the posterior canal of the inner ear is the most commonly affected canal, accounting for 80-90% of cases, followed then by horizontal (5-15%) and anterior canal (1-2%).
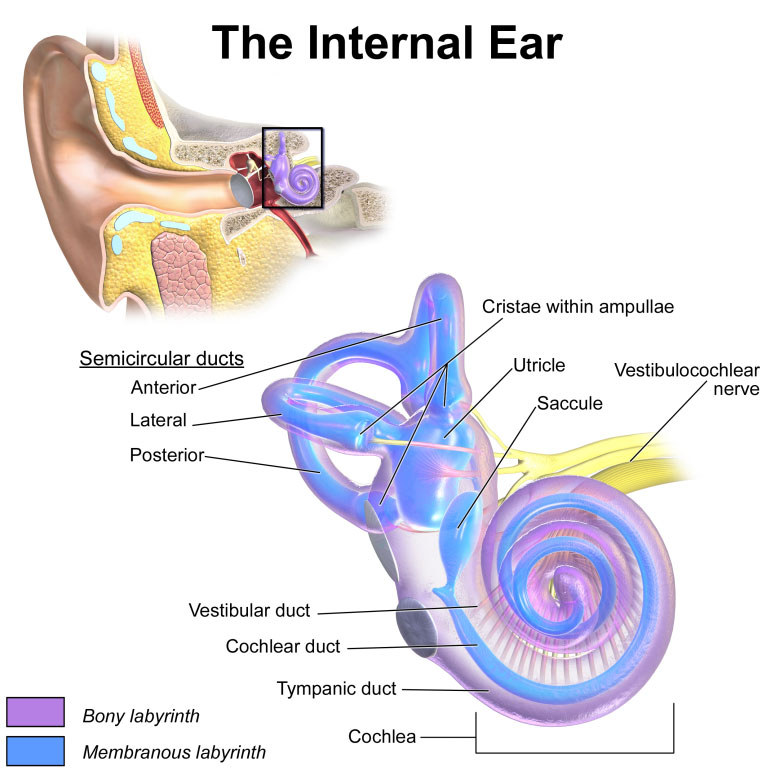
Figure 1 – Anatomy of Inner Ear
“BPPV has an incidence across all age groups of as high as 64 per 100,000. Interestingly, as an individual ages, BPPV becomes more common, rising to an incidence of approximately 10% at 80 years. BPPV affects more women than men, BPPV has a predilection towards women at 2.2 : 1 when compared to men.” (Power et al.)
Falls and falls-related injuries are significantly higher in BPPV patients, than those without BPPV, with “up to 38% experiencing falls as a direct consequence of BPPV, with the incidence of both BPPV and falls increasing with increasing age. The treatment of positional vertigo has been demonstrated to reduce the incidence of falls by 64%.” (Power et al.)
How do we diagnose BPPV?
Commonly BPPV is diagnosed by a test called the Hallpike-Dix Manoeuvre. This test is classed as positive if there is the reproduction of nystagmus. Nystagmus, put simply is the flicking or beating of the eyes from side to side.
It involves the patient starting in a sitting position with their head turned 45 degrees to the side. The practitioner then lowers the patient into a lying position with the neck in a slightly extended position. The practitioner then observes the patient for 30 seconds to confirm or deny the presence of nystagmus or any other vertigo symptoms.
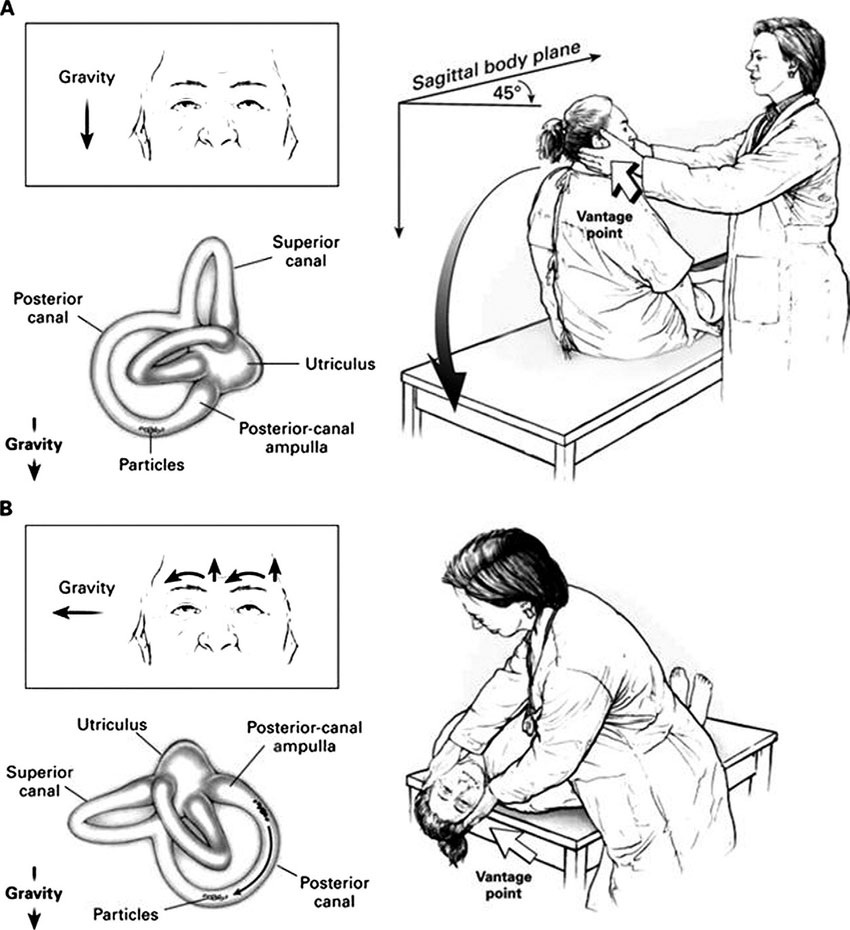
Figure 2 – The Hallpike-Dix Manoeuvre A commonly used test to assess BPPV
Nystagmus can vary, meaning that the eyes can flicker or beat differently. The way the eyes flicker will determine which type of BPPV a person has and where the crystals in the inner ear have travelled to (which canal).
For instance, if someone’s Nystagmus occurs so that there is a slow move to the horizontally to the left and a fast flick horizontally to the right, it can be confirmed that this is a case of right sided, BPPV.
Put simply, the direction of the fast flicker of the eye always indicates the same side that is involved.
How do you treat BPPV?
Physiotherapy can be beneficial for patients with BPPV as it usually responds very quickly to the correct and appropriate treatment. From one study done, “out of 314 patients, 91% percent of people with posterior canal BPPV were treated effectively within 2 sessions or less, using the Epley Manoeuvre.”
The Epley Manouvre is a commonly used treatment used for BPPV. It involves a sequence of positional changes that help to reposition the position of the calcium carbonate crystals in the inner ear back to where they should be in the utricle.
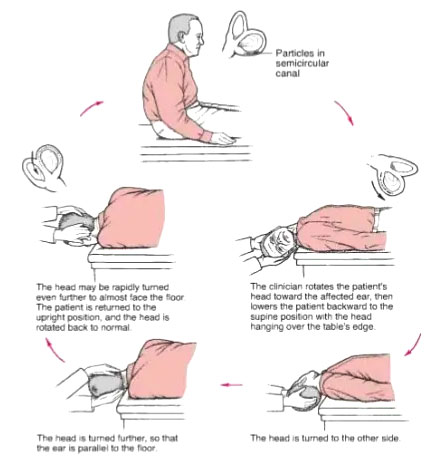
Figure 3 – The Epley Manouvre, used for treatment of Posterior Canal BPPV
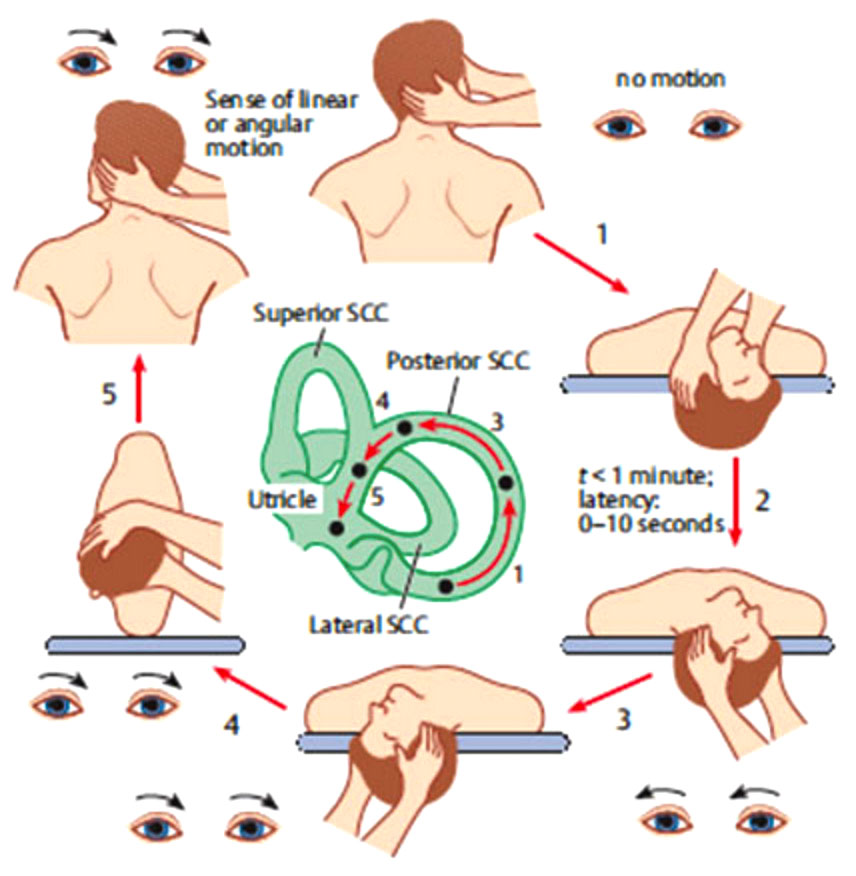
Figure 4 – A representation of what is happening to the crystals in the inner ear during an Epley Manoeuvre.
If you suffer from vertigo, you can also try the Epley manoeuvre at home as a way of self-treatment and prevention.
It is important to ensure that you follow the correct technique and adopt the right head position whilst doing the Epley Manouvre at home to get the best outcome. If done incorrectly it can exacerbate your symptoms. It is important not to drive on the same day as you have done the Epley manoeuvre in case of an exacerbation and danger to yourself and others.
Futhermore, if you are going to see a Physio for BPPV always have someone to drive you to and from the appointment.
References:
Power, L., Murray, K., & Szmulewicz, D. (2020). Characteristics of assessment and treatment in Benign Paroxysmal Positional Vertigo (BPPV). Journal Of Vestibular Research, 30(1), 55-62. doi: 10.3233/ves-190687
Oron, Y., Cohen-Atsmoni, S., Len, A., & Roth, Y. (2015). Treatment of horizontal canal BPPV: Pathophysiology, available maneuvers, and recommended treatment. The Laryngoscope, 125(8), 1959-1964. doi: 10.1002/lary.25138
Shigeno, K. (2017). Positional Down-Beating Nystagmus caused by a variant of Posterior-canal BPPV or Anterior-canal BPPV. Equilibrium Research, 76(6), 684-691. doi: 10.3757/jser.76.684
Bhandari, A., Kingma, H., & Bhandari, R. (2021). BPPV Simulation: A Powerful Tool to Understand and Optimize the Diagnostics and Treatment of all Possible Variants of BPPV. Frontiers In Neurology, 12. doi: 10.3389/fneur.2021.632286
Aso, S., Yasumura, S., Asai, M., Shojaku, H., & Watanabe, Y. (1995). The Effect Of Epley's Maneuver On Benign Paroxysmal Positional Vertigo(BPPV). Equilibrium Research, 54(6), 547-552. doi: 10.3757/jser.54.547
