
Pelvic Organ Prolapse
Despite the fact that Pelvic Organ Prolapse (POP) is becoming increasingly more common, there is seldom discussion of this condition and the impact it can have on a women’s life. Prolapse affects approximately 14-34%(1) of women post-menopause, and its surgical repair is the most common procedure performed in middle-aged women. Although it is not life threatening, POP is a distressing condition that can result in deterioration of bladder, bowel and sexual function(2).
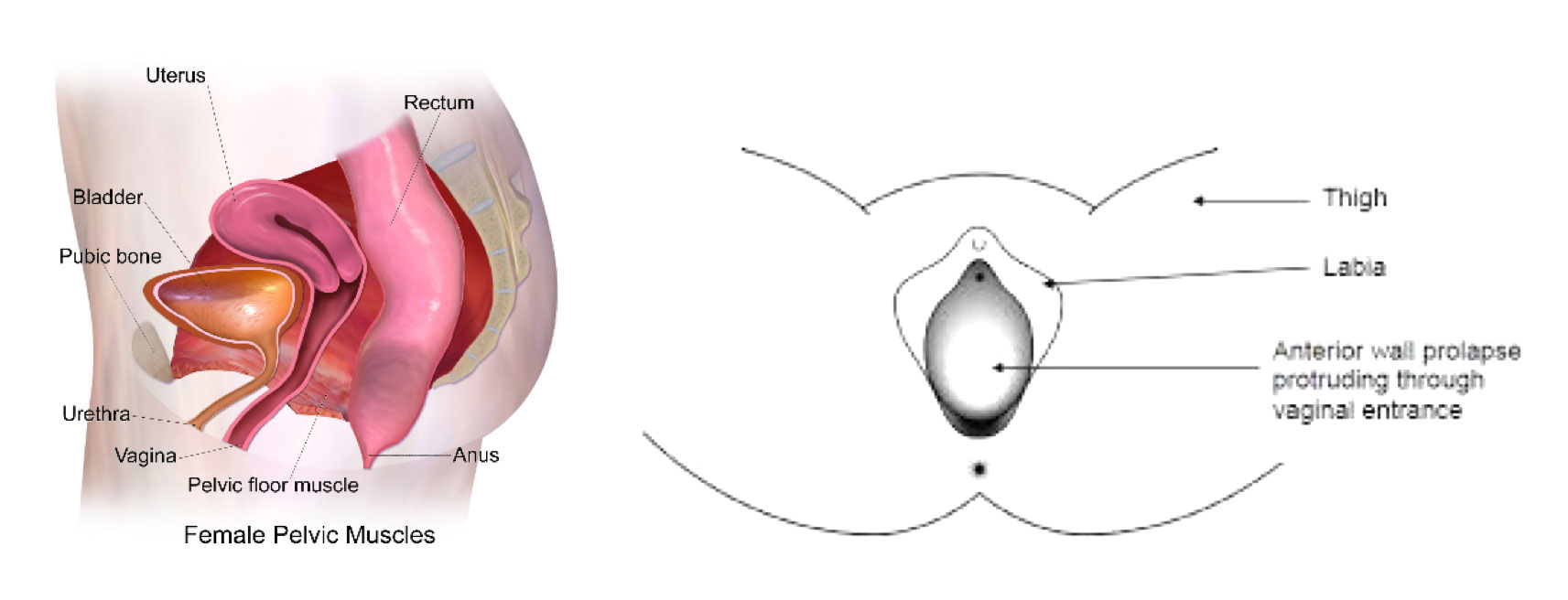
POP occurs when there is a weakness in the supporting structures of the pelvic organs (the bladder, the uterus or womb, and the rectum or bowel). This allows for the downward slippage of any one of these organs towards the opening of the vagina. To explain this further, we first provide some context:
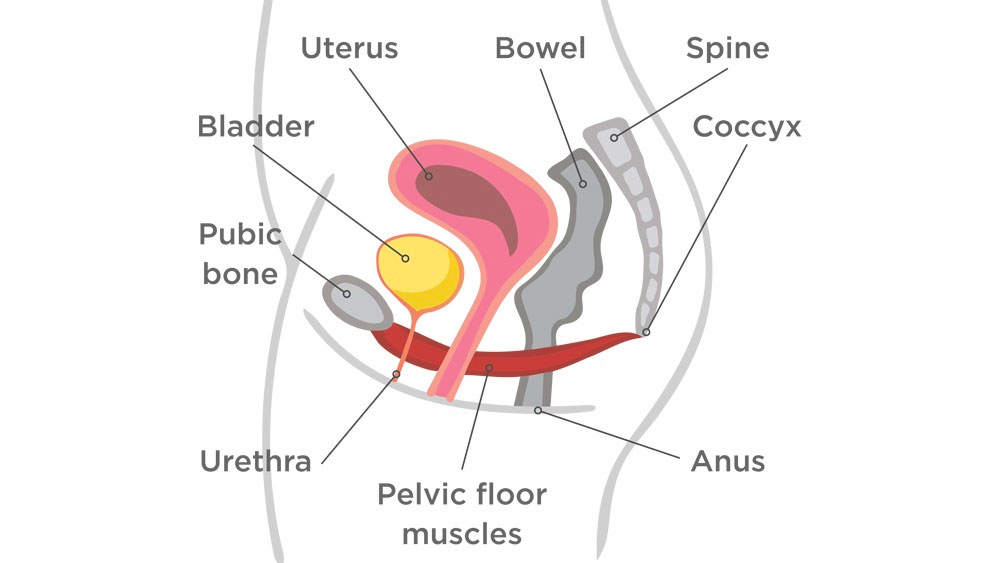
If we picture the pelvic region, we have:
- The bones
3 bones that inter-lock to form a ring shape. Inside this ring is the pelvic cavity. - The pelvic organs
Bladder, uterus (or womb) and rectum (or bowel) that sit inside the pelvic cavity. - The pelvic floor
A sling-like structure of connective tissue and muscles that interplay to support the pelvic organs inside the pelvic cavity. Without both connective tissue and muscular support, the pelvic organs will drop out of the body.
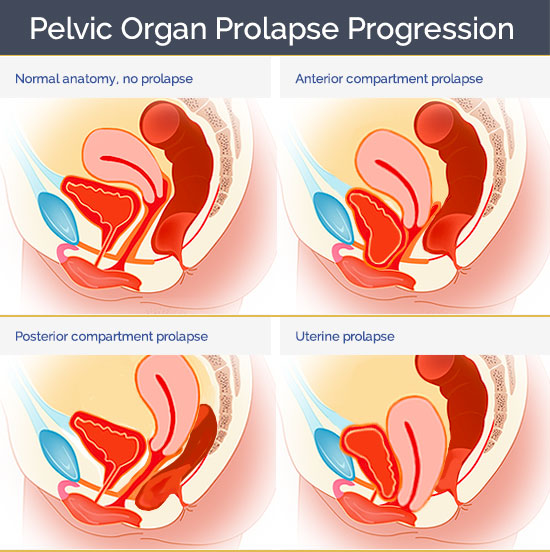
If there is damage to either the pelvic floor’s connective tissue and/or muscles, any combination of the pelvic organs can begin to slip down. Furthermore, the symptoms of prolapse extend into the multiple domains, including physical, mental, social and sexual health. The main symptoms of POP include:
- Discomfort or a sense of “heaviness” or “dragging” in the vaginal region
- Issues with bladder or bowel control and function
- Pain during sex
- Impact of self-esteem and sexuality
Prolapse and Pregnancy
Unfortunately the greatest risk factor for POP is vaginal delivery of a baby(3). The stretch of the soft tissues around the baby’s head can weaken the pelvic floor muscles and/or connective tissue, thus impairing the support of the pelvic organs. However, it is important to remember that:
After birth is a crucial period to potentially prevent or even reverse a woman’s Pelvic Organ Prolapse (POP).
This is one of many reason why a comprehensive post-natal examination is so important prior to returning to activity and sport. Up to 6months following a un-complicated birth, structures of the pelvic floor are still repairing themselves, and thus, are still vulnerable to injury in high impact sports. For example: HITT classes, crossfit, weight lifting or running.
Other factors that can increase risk of POP are multiple births, ethnicity, poor general health, constipation, irritable bowel syndrome(3).
Readiness to Return to Activity
A thorough pelvic floor assessment, as conducted by a Women’s Health practitioner, includes examination of:
- Pelvic floor muscular function,
- Integrity of the pelvic connective tissue, and
- Assessment of any other impacting musculoskeletal issues.
Through this, a health practitioner is able to judge a woman’s risk of POP and decide whether they are safe to return to their given sport.
For general information regarding pelvic organ prolapse (POP), please click the link below to access The Royal Australian and New Zealand College of Obstetricians and Gynaecologists’ pamphlet:
References
1. Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women's Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002 Jun;186(6):1160-6. PubMed PMID: 12066091.
2. Persu, C., Chapple, C. R., Cauni, V., Gutue, S., & Geavlete, P. (2011). Pelvic Organ Prolapse Quantification System (POP-Q) - a new era in pelvic prolapse staging. Journal of medicine and life, 4(1), 75–81.
3. Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL. Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol. 2007 Jun;109(6):1396-403. PubMed PMID: 17540813.
